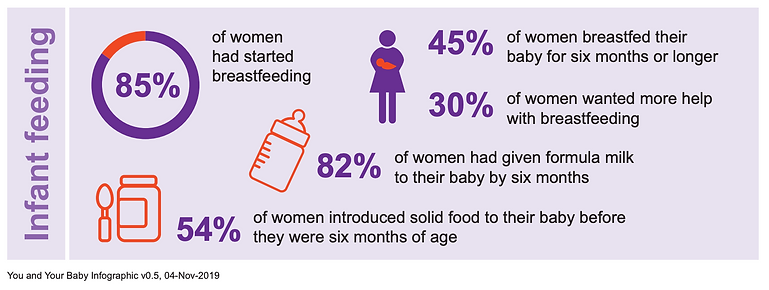
Up until 2010 there was a national survey of infant feeding practices every 4 years, which showed that initiation of breastfeeding was slowly climbing and had reached more than 80%. Smaller National Maternity Surveys since then have shown static initiation rates. Rates of any breastfeeding continue to slowly improve but are still low relative to other countries. Breastfeeding figures from the Department of Health and Social Care have always been lower than the national surveys - both ways of estimating have their weaknesses so the true figure may lie between the two. These two figures and the infographic above are from the 2018 National Maternity Survey. The pandemic did not seem to have a major effect on breastfeeding rates nationally, although there was a reduction in exclusive breastfeeding at six weeks after birth, a sharp rise in parents reporting inadequate feeding support, increased attendance at ED with feeding issues and a rise in postnatal depression and anxiety.
Exclusive breastfeeding/chestfeeding (considering liquids only, not complementary feeds) is around 25% at around 2-3 months of age and 18% at 6 months.
Certain factors are associated with lower initiation and continuation rates - mothers who are more economically deprived are most at risk - for example those in the most deprived quintile had an adjusted odds ratio of 0.68 for breastfeeding initiation. Younger people and smokers also show reduced breastfeeding rates. In general, people from black and minority ethnic groups have higher initiation and continuation rates for breastfeeding, but this may hide significant differences among specific ethnic groups with different historical and cultural attitudes to breastfeeding. Rates are lower in the devolved nations than in England.
There are many reasons for the poor state of breastfeeding in the UK, compared to other high income countries. The UK World Breastfeeding Trends Initiative Report in 2016 identified insufficient training for health professionals as one of seven key gaps.
Figure from WBTi UK, click on the picture to go to the site
What do families say?
The 2017 Scottish Infant Feeding Survey reported that:
-
Two thirds of those who had initiated breastfeeding/chestfeeding reported experiencing some problems
-
Half had difficulty with attachment to the breast/chest in the early days
-
65% were concerned about their milk supply in the first few weeks
-
A quarter said that they had been made to feel uncomfortable when breastfeeding/chestfeeding their baby
-
Three quarters of those who stopped breastfeeding/chestfeeding wanted to continue
-
Of those who stopped breastfeeding/chestfeeding, 77% had problems with attachment to the breast/chest and 86% were concerned about their milk supply
The 2018 National Maternity Survey in England showed that a third of respondents wanted more help with breastfeeding/chestfeeding than they received.
It is also important to note the mental health impact of this steep drop off in breastfeeding/chestfeeding rates. Those who plan to breastfeed/chestfeed and don't succeed have a 50% higher rate of postnatal depression than those who plan to breastfeed/chestfeed and do so. This is a useful website for families and health professionals to work through their feelings about feeding.